JTI research on long-term use of opioids by patients with rib fractures wins two awards
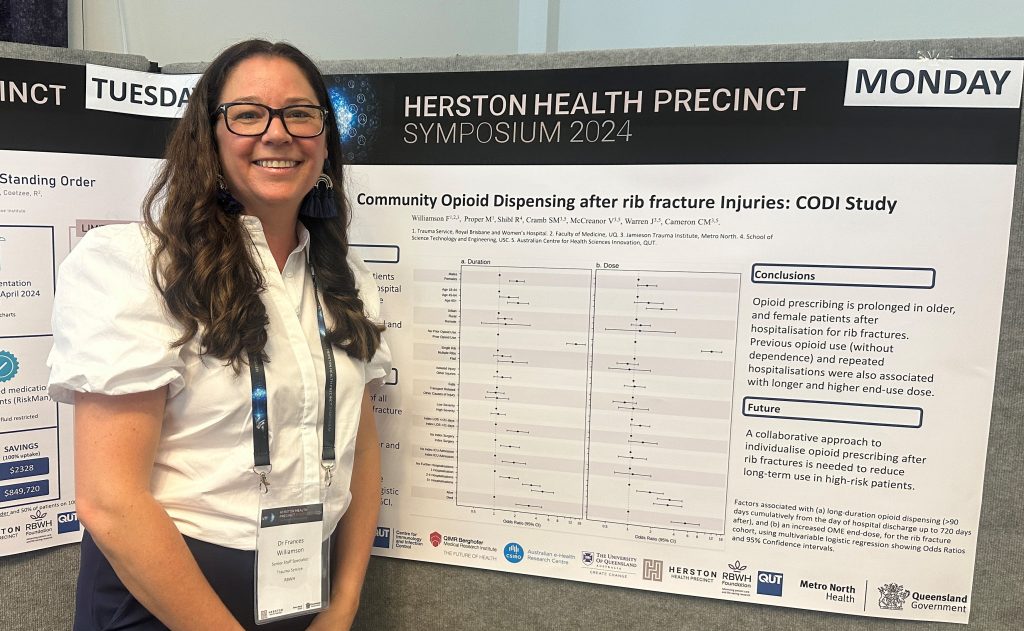
Dr Fran Williamson presenting a poster at the Herston Symposium.
Understanding what happens to our injured patients after they leave hospital is an important area of research which can inform ongoing care. It is known that rib fractures are both common, and painful, and the management focus whilst they are being treated in the hospital is to ensure they have enough pain medications on board to be able to breathe and mobilise in order to avoid complications. The pain relief strategy is often termed ‘multi-modal’ which means a variety of different types of pain relief is used, to help reduce overall reliance on opiate medications.
There is worldwide recognition that opioids can lead to harm, and so any strategies to reduce use are warranted. What is not known is what happens after the patient is discharged home, in particular how long patients require pain relief for. There have been recent studies that suggest that in some patients with rib fractures there is ongoing pain and impact to return to function at 6 months post injury. Our study, led by Dr Fran Williamson and Prof Cate Cameron was focussed on identifying not only how long patients needed pain relief for, but also what factors might contribute to this ongoing need. Our study was the first of its kind to include all adult patients who were admitted to any hospital across Queensland with rib fractures and be able to follow up their opioid use over a two-year period after injury. Conditions that might cloud the use of pain relief medications, such as cancer and patients who were on opioid dependence programs were excluded.
The results, published in the British Journal of Pain, showed that in about half of all patients who were admitted to hospital with rib fractures they needed more opioid pain relief scripts after discharge. Of these patients, a quarter needed ongoing opioid medications beyond 90 days after discharge. Of concern the average length of use in this cohort was 321 days! There was not a significant difference between patients who had single, multiple or flail chest fractures, suggesting that another reason, that is not just severity of injury, was driving the ongoing pain relief use.
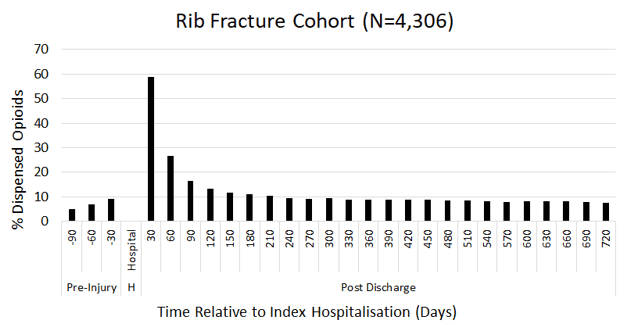
Proportion of persons with rib fracture having opioids dispensed for each 30-day interval, from 90 days pre-injury hospitalisations to 720 after.
The team then performed a multivariate regression analysis and found that older and female patients were at higher risk for ongoing opioid use, and that in addition, if the patient had used opioids in the 3 months prior to their rib fracture admission this also increased the duration. Older age and previous opioid use were also associated with increasing dose requirements at 2 years post injury.
Further studies are required to explore these factors in more detail, and engagement with community services to ensure shared understanding are required.
Fran was excited to present these important findings at the Australia and New Zealand Trauma Society conference in Brisbane in October and won the best oral medical paper for the presentation. She also won an abstract prize for the study presentation at the University of Queensland Faculty of Medicine Research Day in November. Well done Fran and all the research team!
Dr Fran Williamson receiving the best oral medical paper at the ANZTS Conference.
