HBI Anaesthesia and Intensive Care Enhances Medical Training with Near-Zero Waste 3D printing at ANZCA Conference
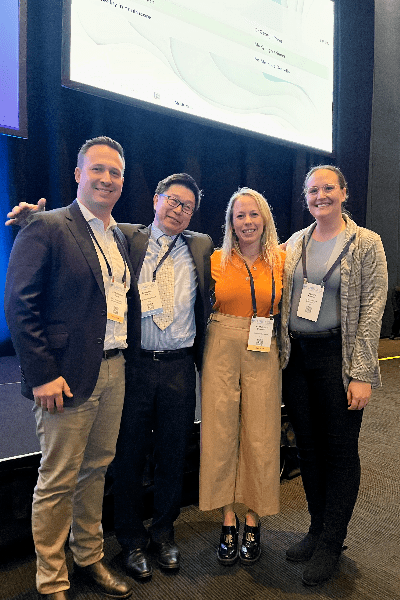
Brisbane, Australia – In a showcase of innovation at the Australian and New Zealand College of Anaesthetists (ANZCA) Annual Scientific Meeting (ASM) in May 2024, HBI Anaesthesia and Intensive Care unveiled the transformative potential of 3D technology in medical training. Led by RBWH anaesthetists Dr George Pang and Dr Chris Futter, alongside HBI engineer Ryan Daley, the team demonstrated how 3D modelling and printing can be implemented by anaesthetics departments in hospitals.
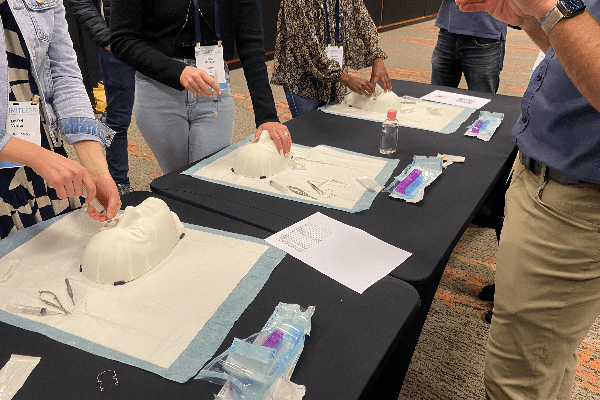
The team’s expertise lies in harnessing 3D modelling and printing to create advanced training and simulation models that complement traditional skills development methods. These 3D models, such as the 3D printed front-of-neck access trainer and the extracorporeal membrane oxygenation (ECMO) model, offer advanced anatomical accuracy and haptic feedback. Moreover, they are designed for sustainability, with Dr Pang highlighting their near-zero waste approach: “In our airway access model, the rigid bust and trachea are 3D printed with tough materials that withstand transport and cleaning. Soft neck inserts are created using ballistic gel casted in 3D printed moulds. Those gels are remoulded and reused indefinitely.”
At the ANZCA ASM themed “Limitless,” the HBI team hosted a “3D manufacturing for critical care” workshop, offering 10 attendees insights into the latest clinical and engineering advances. Dr Pang, Dr Futter, along with engineers Ryan Daley and Dr David Forrestal, guided the participants through image segmentation, 3D modelling of anatomy, and selecting optimal printing techniques and materials. In a separate session, Dr David Fung, Dr Chris Futter, and Ryan Daley, along with colleague Dr Conrad Macrokanis, hosted a workshop on regional anaesthesia training for 24 participants, using a 3D printed eye block trainer designed with haptic feedback and cost-effectiveness in mind. “The 3D printed eye block allows participants to experience and learn needle insertion skills that are traditionally regarded as difficult to comprehend, acquire and maintain,” explained Dr Futter. “We also are working on a companion virtual reality app to get up close with the anatomical structures associated with the eye block”. “I feel more confident to safely perform peribulbar blocks after this session” confirmed one of the participants.
In addition, Dr Futter co-chaired the “Amazing technology in healthcare” session, where Dr Pang shared how the team employs 3D technology to problem-solve challenges in anaesthesia practice. UQ MD-PhD candidate Kyleigh Kriener shared her research on biomechanical measurements from human tissues for medical skills development, while HBI General Manager Mathilde Desselle discussed the design of interactive virtual reality experiences in healthcare, with applications in pain management, rehabilitation and visualisation.
The HBI Anaesthesia and Intensive Care team’s pioneering work with 3D printing represents a significant step forward in medical education, offering clinicians unprecedented access to high-fidelity and affordable training tools.