HBI hosts UQ Medical Device Engineering student projects
Students enrolled in BIOE6901: Medical Device Engineering at the University of Queensland with Dr Alejandro Melendez-Calderon were introduced to HBI workflows to investigate solutions for clinically applied 3D technologies. This is the second year HBI has hosted students from this course and looks forward to future engagement with the students and course.
Digitised Measuring and Monitoring of 3D Printed Medical Devices
Group members: Gabrielle Byrne, Claire Careless, Yu-Zhen Eva Seet
Supervisor: Dr David Forrestal, Jacob Skewes, Isabel Byram
3D printed anatomical models are an increasingly used for the purposes of education, surgical training and procedural planning due to its accuracy, ability to match patient-specific anatomy, and range of materials that can replicate complex tissue properties and architecture (Baskaran et al., 2016). 3D printed models allow surgeons to visualise patient anatomy tangibly that cannot be achieved solely through standard medical imaging techniques. Surgeons can then use these models to plan and prepare for complex surgical procedures, identify challenges, and decide on the surgical approach to be taken. As the models can be printed to patient-matched specifications using CT or MRI imaging, surgeons can tailor the procedure to the patient’s variations in anatomy, ultimately resulting in improved surgical precision and reduced operating time, improving patient outcomes.
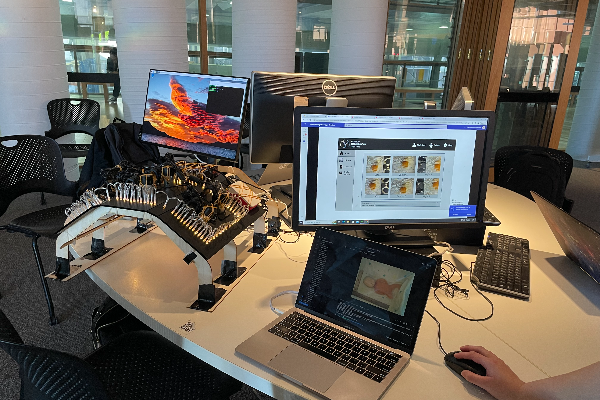
The prototype delivered along with this report is capable of processing images of a 3D printed model taken throughout the printing process into binary images, extracting dimensions from the images and comparing to respective dimensions extracted from the associated CAD model.
The intended purpose of the device is to act as a Validation tool for external measurements of a simple 3D printed anatomical models for procedural planning, with an approved CAD model, printed in an Ultimaker S3 3D printer, utilised by biomedical engineers who print the models.
The device is exempt from TGA classification as although it takes patient anatomical information from a CAD model, it does not take data directly from a medical device, is it intended for the purpose of providing a recommendation to a health professional (whether the model is compliant with dimensional specifications), and is not intended to replace the clinical judgement of the health professional, as it is based on information that can otherwise be verified (Therapeutic Goods Administration, 2021).
Future applications for this device are potent and include the ability to station 3D printers within metro and rural hospitals alike, so that doctors are able to produce models on site after obtaining a model file digitally, without requiring a validation engineer. This technology may also be applied to automate rapid production and validation of patient matched implants and prosthetics, driving down the cost of custom surgical implants.
Baskaran, V., Štrkalj, G., Štrkalj, M. & Di Ieva, A. 2016. Current Applications and Future Perspectives of the Use of 3D Printing in Anatomical Training and Neurosurgery. Frontiers in Neuroanatomy, 10.
Smooth and Transparent Facial Orthosis
Group members: Alyssa Binder, Ben Colbert, Febrian Kachina, Yang Zhang
Supervisor: Dr David Forrestal, Roozbeh Fakhr, Isabel Byram
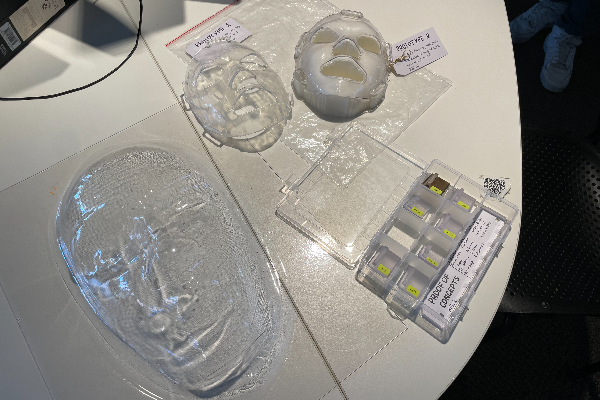
The primary intended purpose of a Transparent Facial Orthosis (TFO) is to prevent damaged skin tissue from scarring after a patient receives extreme facial burns, typically third-degree and above. The orthosis provides a consistent, gentle source of pressure application to facilitate scar tissue remodelling whilst maintaining patient anatomical contours to prevent excessive scar contracture. The orthosis creates a blanched effect over the scar, indicating flattening of the surface and minimizing blood flow to reduce inflammation and preserve damaged tissue. Along with this, the TFO also protects fragile maturing scar tissue from irritants and unwanted shear forces that may impair the healing process.
At HBI a 3D-printed, patient-specific compression mask tailored to minimise the patient epidermis from scarring. Whilst the production of a TFO to minimise the risk of tissue scarring is viable and, on the market, HBI seeks to improve the medical device production process in promoting smoothness and transparency. These are both critical qualities of facial orthosis, as transparency provides a clearer view of skin condition for clinical outcome determination and yields a less confronting nature which promotes patient outcomes through compliance with recovery activities. The smoothness of the mask is critical for minimizing the risk of infection through providing an easier surface to clean, whilst it also minimizes hazards associated with the daily usage of device.
Photogrammetry Rig for Neonatal Infants
Group members: Ximeng Zhang, Xinyuan Liu, Kayla Wong, Ke Xu, Peter Storeshaw
Supervisor: Isabel Byram, Dr David Forrestal
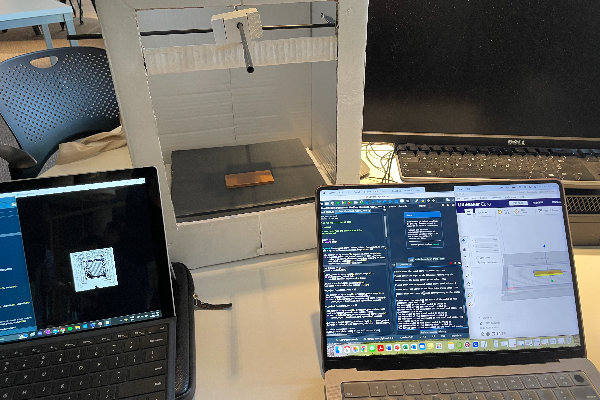
Our team was approached by HBI to find a better way of creating 3-D images of the infant’s face. HBI and clinicians at the Royal Brisbane and Women’s Hospital (RWBH) are undergoing a study to find out if certain facial types are more likely to be injured and how those injures progress. Currently an Artec Leo 3D Hand-held scanner is used to create 3-D models of the infant’s face.
Due to infants needing to remain in an incubator (Kotecha et al., 2015), the current process may disrupt the infants’ care. The movement of the infant during the scan can impact the quality of the resultant image. The infants are currently scanned during cares when the infant is moved and tended to as part of their care plan (Al-lawama et al., 2018). If the study is successful HBI and Dr Mellissa Lai from the RBWH believe that the 3-D scans can be used to create custom masks for infants that are likely to be injured by the current mask.
Al-lawama, M., Alkhatib, H., Wakileh, Z., Elqaisi, R., AlMassad, G., Badran, E., & Hartman, T. (2018). Bubble CPAP therapy for neonatal respiratory distress in level III neonatal unit in Amman, Jordan: a prospective observational study. International Journal of General Medicine, Volume 12, 25–30. https://doi.org/10.2147/ijgm.s185264
Kotecha, S. J., Adappa, R., Gupta, N., Watkins, W. J., Kotecha, S., & Chakraborty, M. (2015). Safety and Efficacy of High-Flow Nasal Cannula Therapy in Preterm Infants: A Meta-analysis. Pediatrics, 136(3), 542–553. https://doi.org/10.1542/peds.2015-0738