JTI Newsletter – November 2025
Contents
Welcome
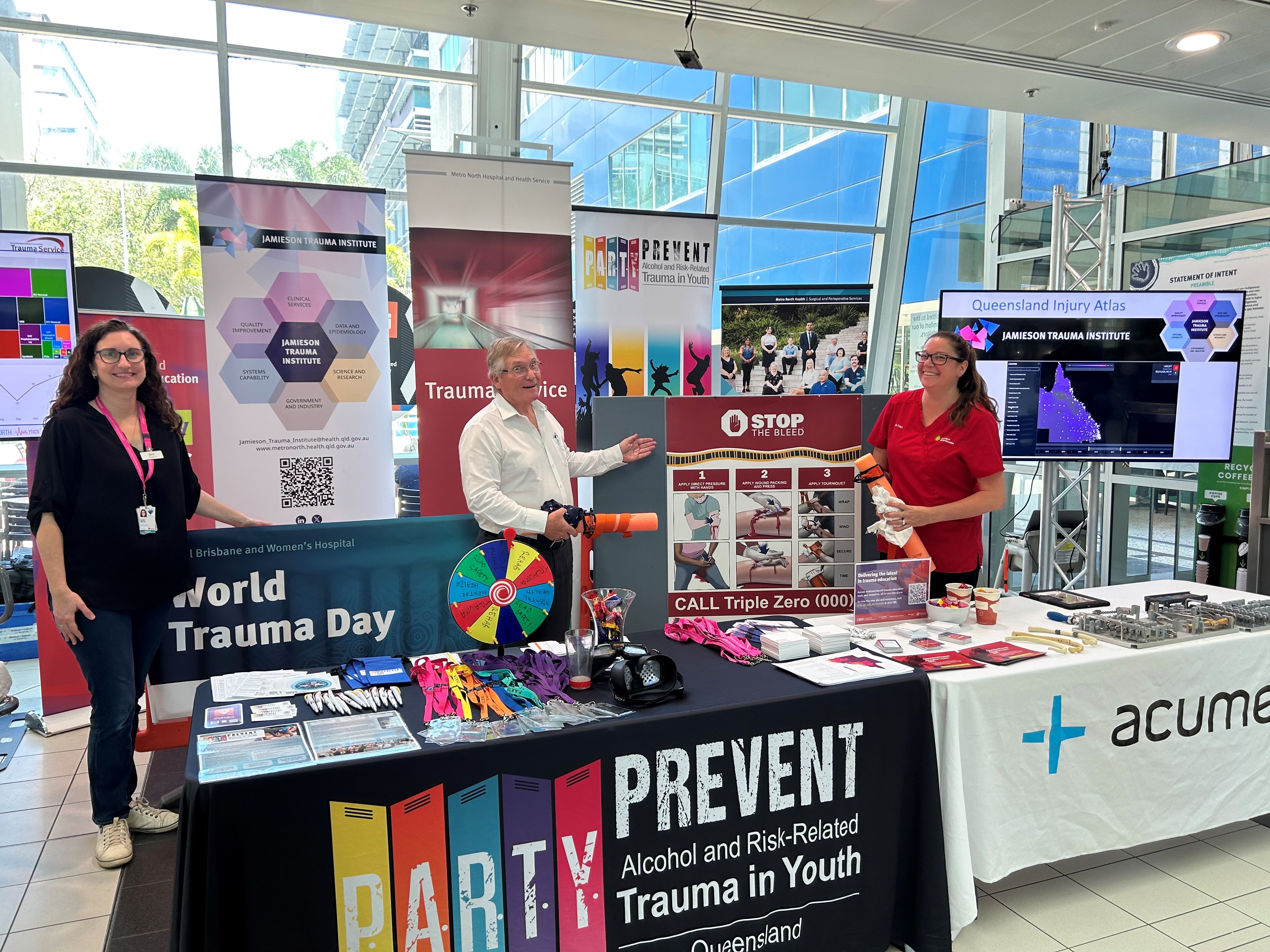
If we thought September was a busy month for the JTI team, October seemed to be over in a blink of an eye! On Friday 17th, we joined forces with the RBWH Trauma Service, Prevent Alcohol and Risk Related Trauma In Youth (P.A.R.T.Y.), Queensland Trauma Education (QTE), and Teamwork and Collaborative Training (TACT) for World Trauma Day. On this day, we aim to raise awareness and promote innovation in trauma care and prevention. Those that spun the wheel and answered their ‘trauma trivia’ question correctly won a chocolate – learning + chocolate = success! We joined workshops and educational programs on trauma prevention and care organised by communities around the world. You can read more about the history and importance of World Trauma Day here.
We also celebrated with Sarah Pearce, who was acknowledged for her service to the Australia New Zealand Trauma Society (ANZTS), and with Dr Rebekah Young, who was awarded the Best Medical Oral Presentation, at the Trauma 2025 Conference in Wellington, 22nd – 24th October. Keep reading for a full wrap-up from the Conference.
Multidisciplinary Trauma Forum: Pre-conference workshop ignites discussion ahead of the ANZTS Trauma 2025 Conference
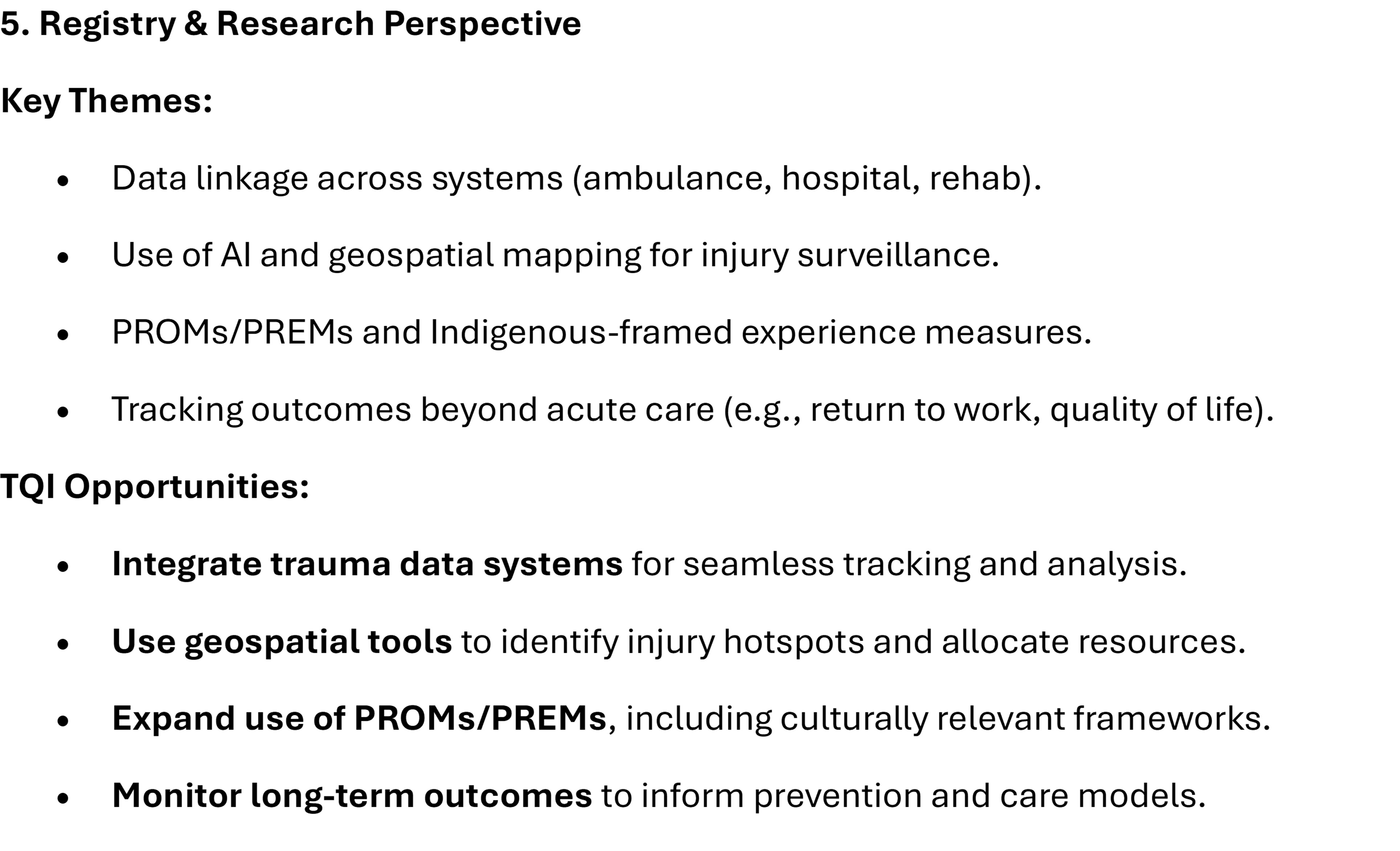
Over 120 delegates attended the Multidisciplinary Trauma Forum, with paramedicine, nursing, medical, allied health, government, registry and research all represented. Jacelle Warren was proud to be part of the organising faculty, with the program full of engaging invited speaker sessions and a rapid-fire session that showed the breadth and depth of trauma quality improvement (TQI), education and research initiatives happening across Australia and New Zealand. Jacelle also chaired the focussed discussion session, which created great conversations about where we need to focus our effort as a trauma ‘whānau’ (Māori word for ‘family’) to improve outcomes for our trauma patients. The discussion summary from the Registry & Research perspective (below) clearly shows the alignment between need, and JTI’s vision.
Beyond acute care: Quantifying hospital sub-acute care and readmission patterns following injury is critical for systems improvement
On Day 1 of the ANZTS Trauma 2025 Conference, Prof Kirsten Vallmuur outlined the need to capture data on sub-acute care and readmissions following transport-related injuries, which are often overlooked in standard hospital trauma registries. By analysing data from almost 90,000 patients hospitalized in Queensland between 2011 and 2020 and following them up at 31-days, 90-days and 1-year post-discharge, Kirsten’s team found that 35% of initial hospital bed-days occurred in sub-acute care, and 17% of patients were readmitted – 42% of these within 31 days. These findings revealed the substantial, ongoing healthcare burden of injury recovery and highlighted the importance of comprehensive data-linkage beyond the acute-care stay to inform better resource allocation and trauma care planning.
International standardisation of patient reported outcome measures for major trauma patients – where are we now?
The ICHOM Set of Patient-Centered Outcome Measures for Major Injury has now been completed, and is the result of dedicated work by a group of leading physicians, academics, and patients. Prof Michael Schuetz presented the list of outcomes that were found to matter most to patients with experience of major injuries. We urge all providers around the world to start measuring these outcomes to better understand how to improve the lives of their patients. See the recently published paper in The Lancet eClinicalMedicine here.
Prof Michael Schuetz presenting the international consensus on major trauma outcome measures at the ANZTS Trauma 2025 Conference
Integrating psychosocial care into trauma surgical training
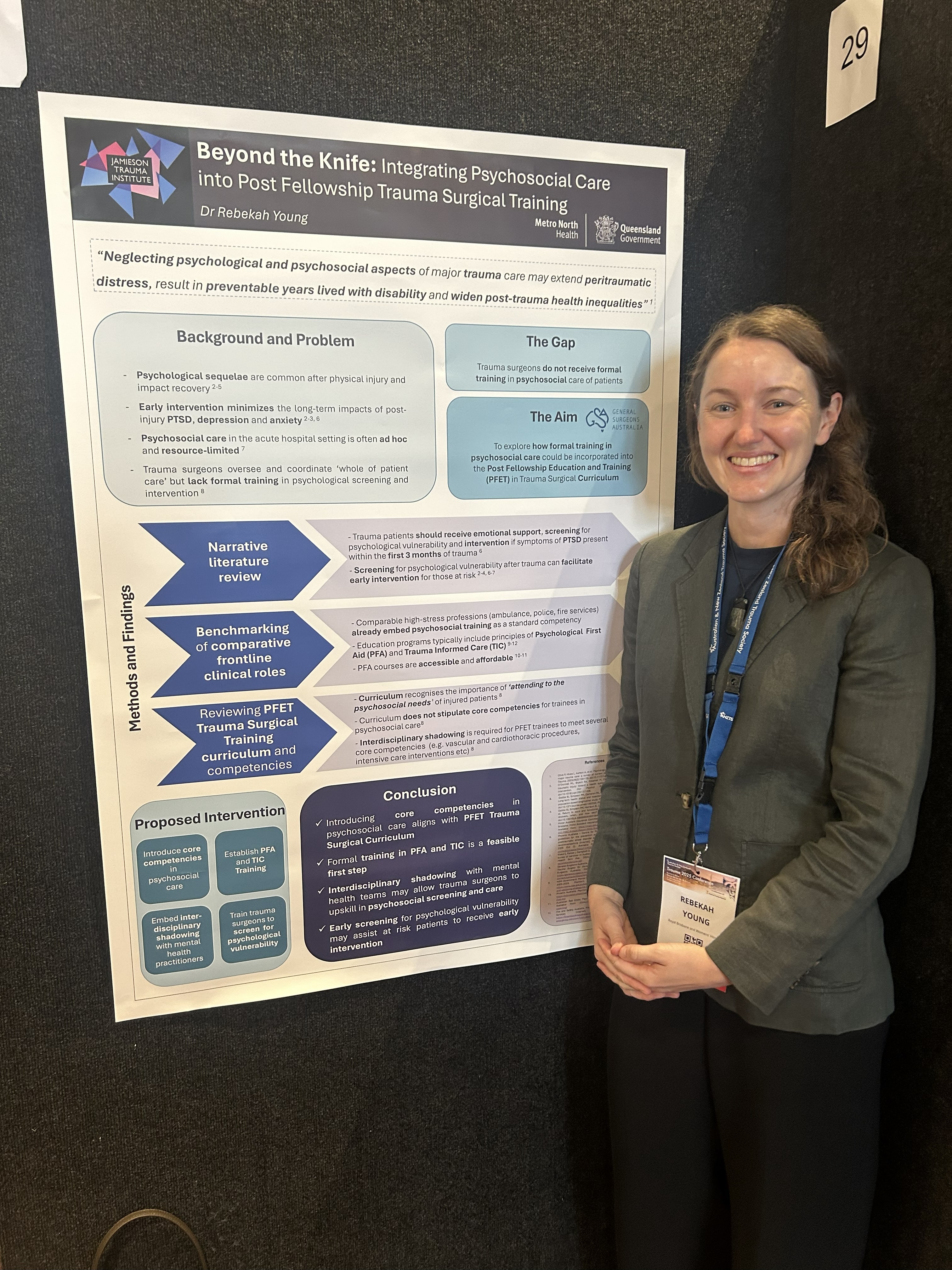
Dr Rebekah Young presenting her poster at ANZTS Trauma 2025 Conference.
Trauma care extends beyond physical injury. Psychological distress after trauma is common, yet formal psychosocial training is absent from current trauma surgical education. Dr Rebekah Young reviewed evidence and benchmarked other high-stress professions, finding that early screening and support improve recovery. Integrating competencies in Psychological First Aid and Trauma-Informed Care within the Post Fellowship Trauma Surgical Curriculum could equip surgeons to recognise and respond to psychological vulnerability. Embedding psychosocial training represents a feasible and necessary step toward holistic, patient-centred trauma care.
How does Queensland’s Trauma System compare?
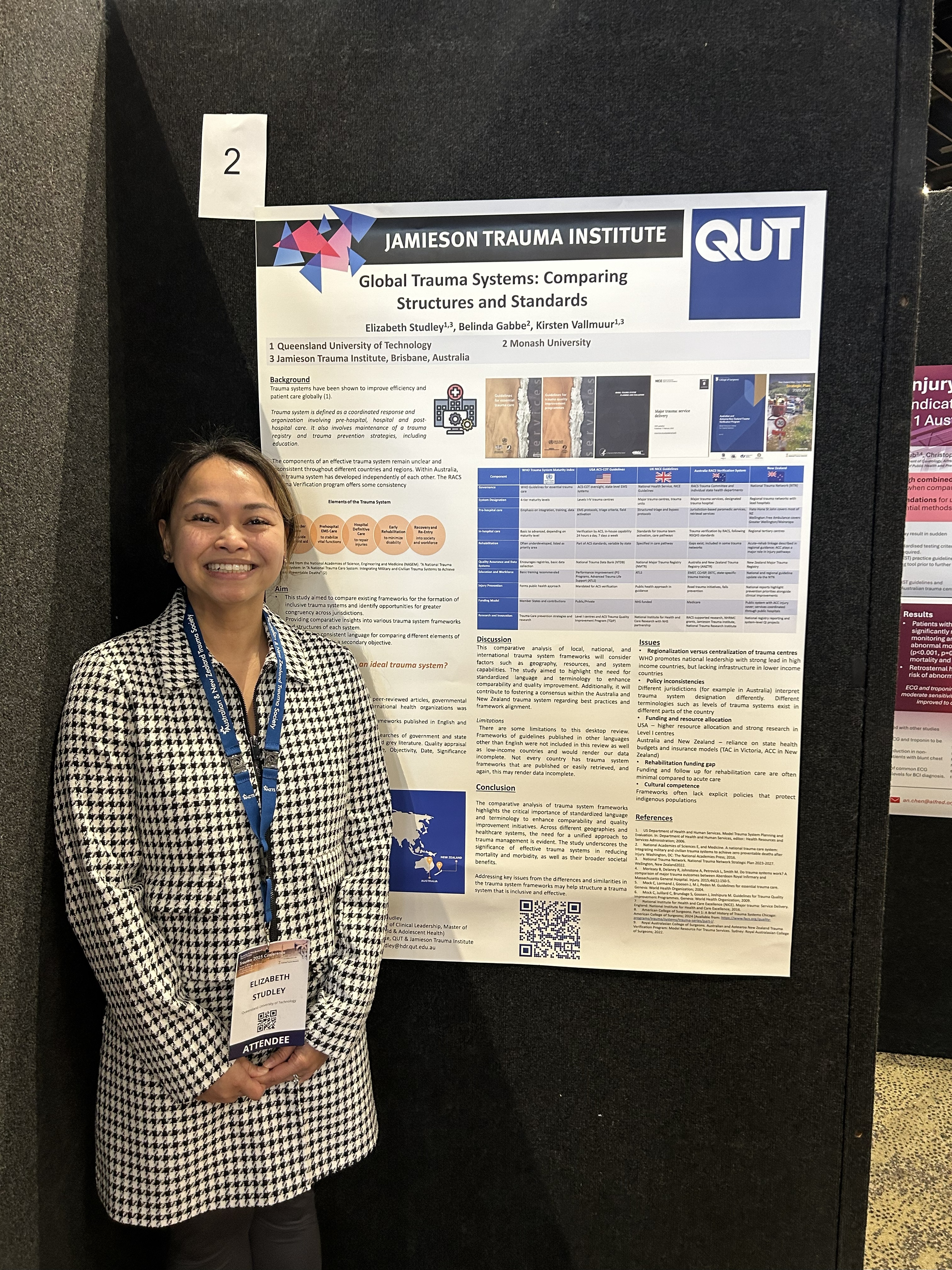
Dr Beth Studley presenting her poster at ANZTS Trauma 2025 Conference.
Dr Beth Studley’s study compared global trauma system frameworks to identify opportunities for greater alignment across jurisdictions. Trauma systems, adapted from military models, are vital for reducing injury-related mortality and morbidity. A literature review of English-language sources revealed diverse approaches, including WHO, US, UK, New Zealand, and Australian state-specific guidelines. Key differences exist in system levels, service provision, and terminology. The analysis underscores the need for standardised language and consistent structural definitions to improve comparability and resource allocation. Establishing a unified framework can enhance trauma care quality, facilitate benchmarking, and support better outcomes for individuals affected by trauma injuries.
JTI data team highlight valuable insights at ANZTS Trauma 2025 Conference
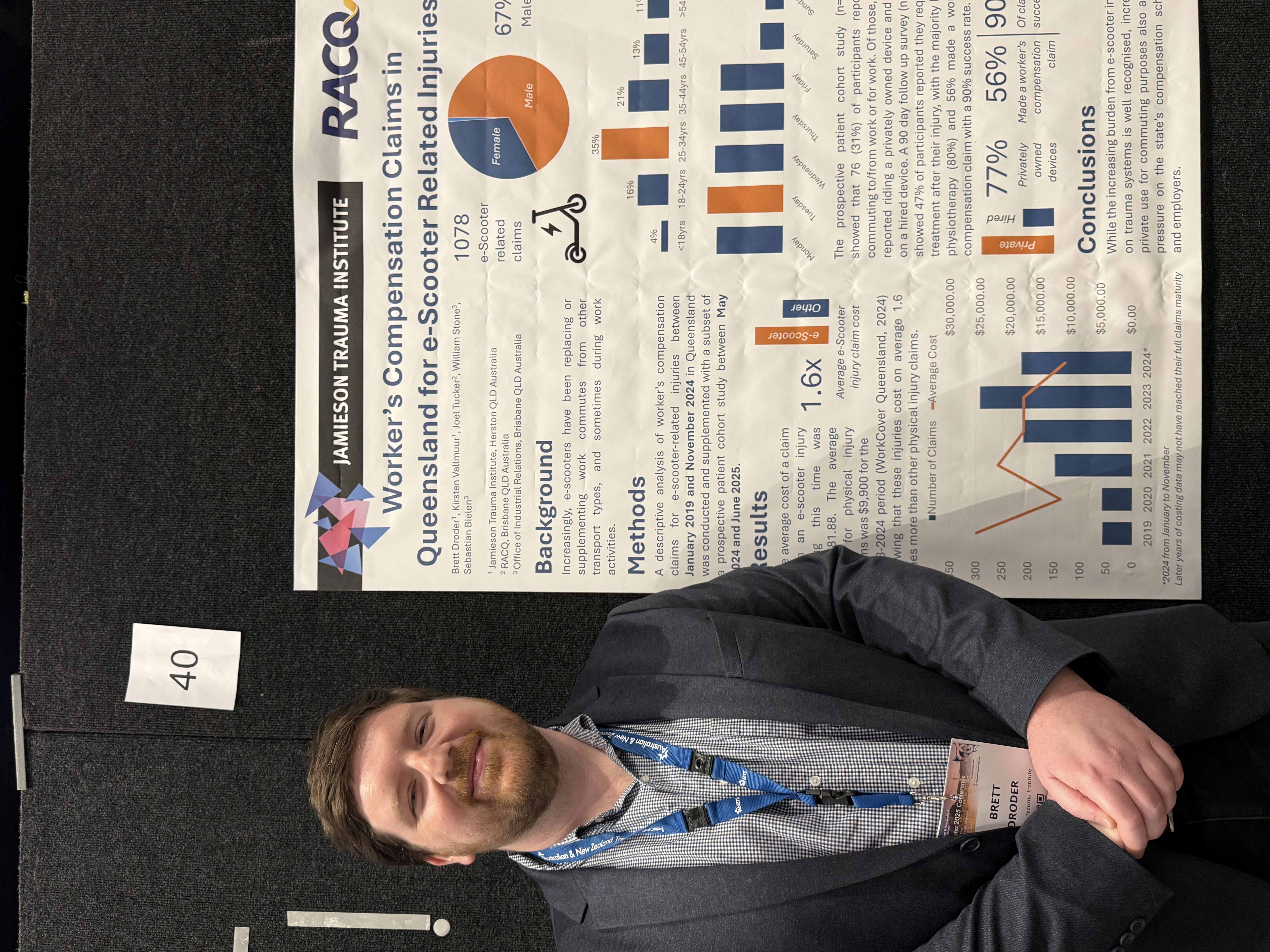
Increasingly, e-scooters have been replacing or supplementing work commutes from other transport types. Brett Droder presented a descriptive analysis of worker’s compensation claims for e-scooter-related injuries between January 2019 and November 2024 in Queensland and supplemented this with a subset from a prospective patient cohort study. The average cost of a claim from an e-scooter injury during this time was 1.6 times more than other physical injury claims in the 2023-2024 period. While the increasing burden from e-scooter injuries on trauma systems is well recognised, increasing private use for commuting purposes also applies pressure on the state’s compensation schemes and employers. In the same week, at the 2025 Australasian Road Safety Conference, Joel Tucker from RACQ presented the same findings as a co-author, and as a part of JTI and RACQ’s broader collaboration on personal mobility device injuries.
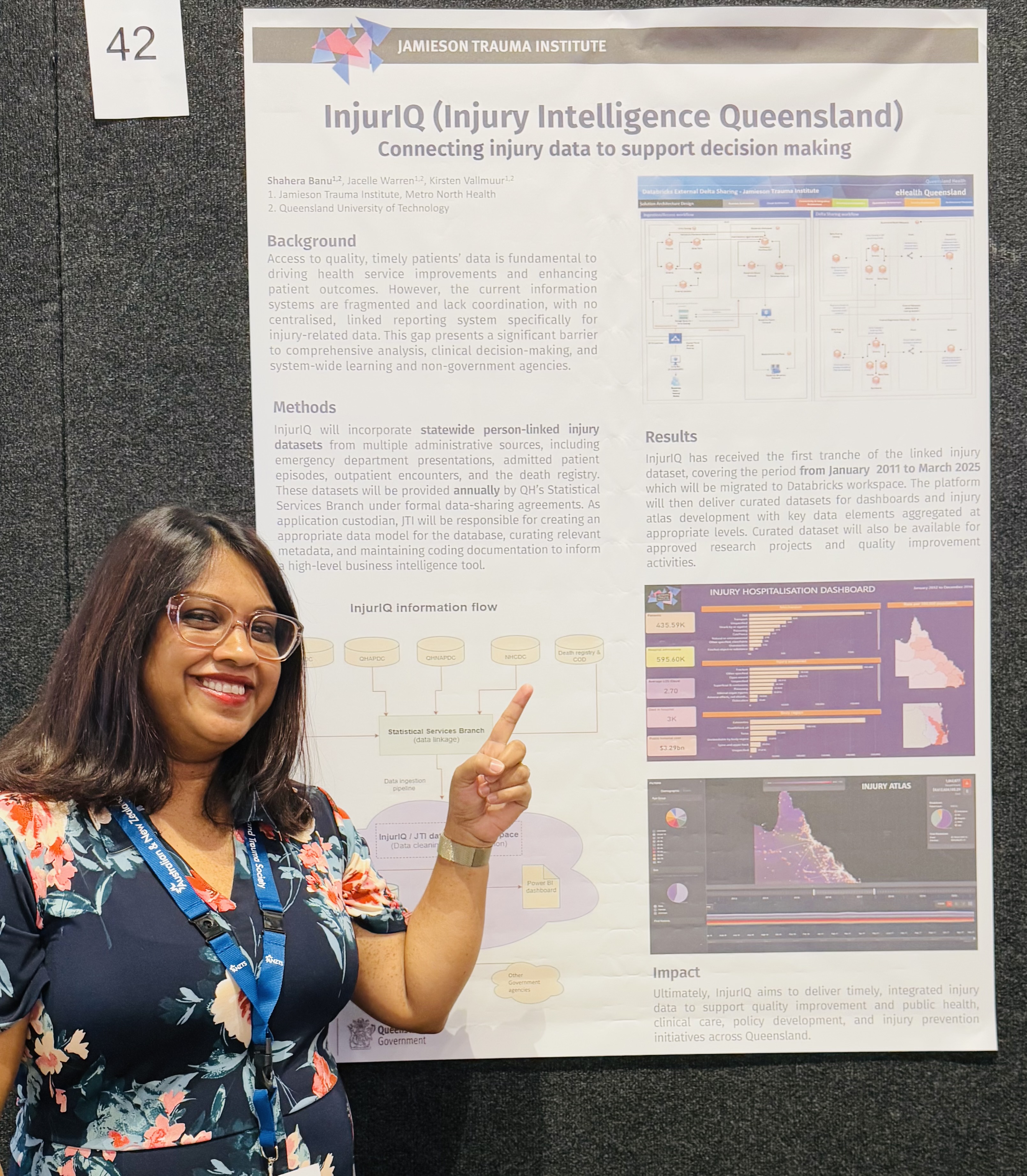
Dr Shahera Banu presented the prototype of InjurIQ, a cloud-based data platform hosted by Queensland Health, developed by JTI to address the fragmentation of injury-related data systems. By integrating person-linked data from emergency departments, hospital admissions, outpatient services, and death registries, InjurIQ enables timely, centralised access to critical health information. JTI oversees the platform’s data model, metadata curation, and coding documentation to support advanced business intelligence tools. The system delivers curated datasets and dashboards for clinicians, policymakers, and researchers, enhancing clinical audits, research, and quality improvement. InjurIQ ultimately aims to improve public health, clinical care, policy development, and injury prevention across Queensland.
Finally, Dr Gi Young Seo presented on the accuracy of ICD-10 coding for acute compartment syndrome, focussing on admissions to Royal Brisbane and Women’s Hospital from 2017 to 2021. Of 246 cases coded as compartment syndrome, only 13% met clinical criteria. Many misclassified cases involved falls with prolonged immobility, rhabdomyolysis, or trauma without compartment syndrome. True cases were predominantly male (83.9%), average age 40.8, and most underwent fasciotomy. Notably, standing-height falls accounted for half of fall-related cases. Findings highlight limitations in ICD-10 coding and suggest that non-traditional injury mechanisms warrant clinical vigilance. Improved data classification methods are needed to enhance injury surveillance and patient care across Queensland for these types of injury mechanisms.
Delays to emergency theatre access – a call to action from Dr Rebekah Young
Dr Rebekah Young’s presentation highlighted a critical system gap in emergency surgical care. Analysing over 1,600 trauma cases at a Queensland tertiary trauma centre, Dr Young found that delays to emergency surgery consistently increased complication rates and hospital length of stay across all injury subtypes. Unlike elective surgery—where waiting times are publicly reported and linked to performance targets—emergency surgery operates without comparable oversight. The findings suggest that these delays carry significant clinical and system costs, underscoring the need for greater transparency, accountability, and process reform to ensure timely access to emergency theatre.

Dr Rebekah Young presenting her award-winning presentation at the ANZTS Trauma 2025 Conference
The $1M Question – What’s the most critical challenge in trauma care today?
Trauma care is at a crossroads—and resources are finite. The last session of the ANZTS Trauma 2005 Conference, chaired by JTI’s Professor Kirsten Vallmuur and NZ Professor Shanthi Ameratunga, and moderated by NZ Professor Bridget Kool, saw a high-energy, thought-provoking shark-tank style plenary, with four leaders in the field taking the stage to pitch their case for what they believe is the most urgent, game-changing challenge facing trauma care today. JTI Director, Prof Michael Schuetz, presented the case for investment in AI & robotics for ensuring a smarter trauma system. The “Shark Panel” (Prof Avery Nathans, Prof Belinda Gabbe, Prof Ian Civil and Prof Martin Wullschleger) asked the hard questions but ultimately, it was the audience who decided which challenge was most deserving of immediate investment and innovation, with the Equity Now pitch led by Associate Professor Courtney Ryder providing such a compelling case the audience were won over. Which challenge would you have chosen to give the money to?:
- The most critical challenge in trauma care is engaging with society. James Hamill
- AI & robotics: Investing in a smarter trauma system. Michael Schuetz
- Equity now: Closing the Gap in trauma outcomes. Courtney Ryder
- The politics of bleeding: funding, policy, and the fight for trauma resource. Rob Harley
PhD student success at International Data Week 2025 conference

Tasmiah Sad Sutopa with principal supervisor A/Prof Susanna Cramb.
Congratulations to JTI/AusHSI PhD student Tasmiah Sad Sutopa for receiving joint second place in the 3-Minute ‘Pitch Your Research’ Competition at the International Data Week 2025 Conference! Tasmiah presented her work on analysing community opioid dispensing trajectories among injured patients using linked administrative data from the Community Opioid Dispensing after Injury (CODI) dataset. From Tasmiah:
“I was honoured to be awarded second place in this competition, which provided an excellent opportunity to represent AusHSI, JTI and QUT among an international community of data scientists and health researchers. I had the opportunity to share my research with a global audience, learn from leading experts in data science, and connect with inspiring early-career researchers from around the world”.
Spotlight on Prof Michael Muller: Stop the Bleed®
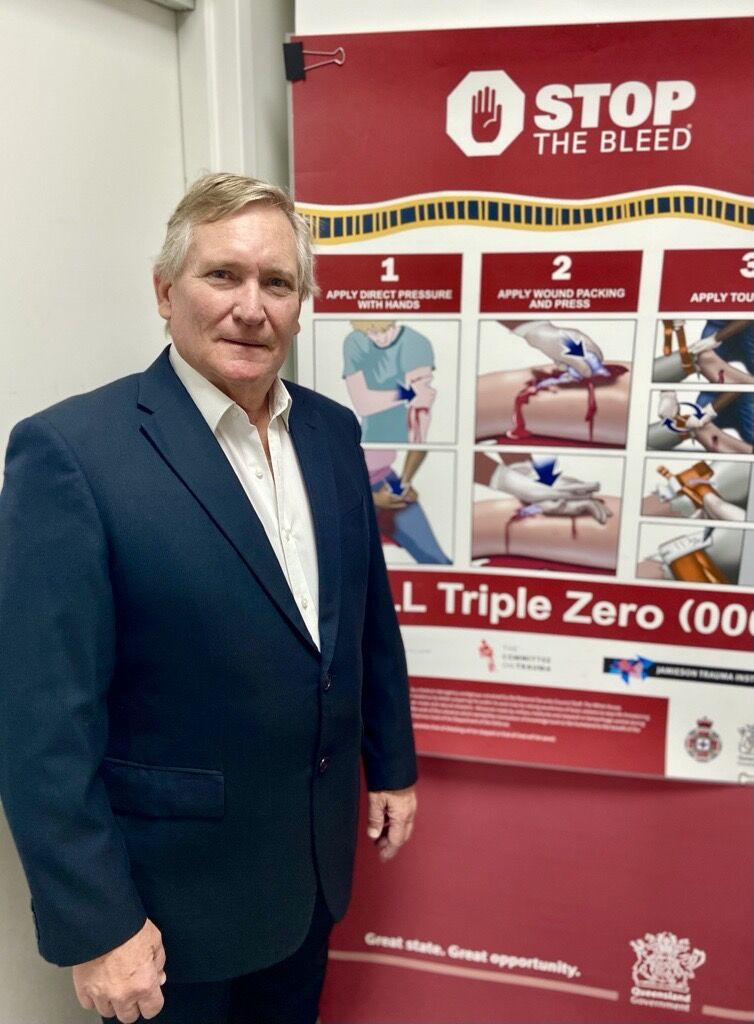
Professor Muller, courtesy of Metro North Health
If you came across a life-threatening accident, would you know how to stop the bleeding? 🩸🩸🩸
Professor Muller and the team at Jamieson Trauma Institute bring life-saving programs such as Stop the Bleed® to Queenslanders from all walks of life.
Professor Muller, who works as a burn and trauma surgeon at RBWH, also co-leads education and training at JTI and plays an important role in guiding research to educate our ever-growing population.
Stop The Bleed® courses train the public to save lives through some basic actions to stop life-threatening bleeding following emergencies. It’s the first time Australians have been able to access this type of training , which was created by the American College of Surgeons and now runs through the Queensland Ambulance Service and JTI.
With over 4,000 people trained so far in high schools, regional centres, and remote indigenous communities across the state, Professor Muller is hopeful that 60 percent of Queenslanders will know about Stop the Bleed® by 2032.