Optimising dosing of antimicrobials in ECMO patients
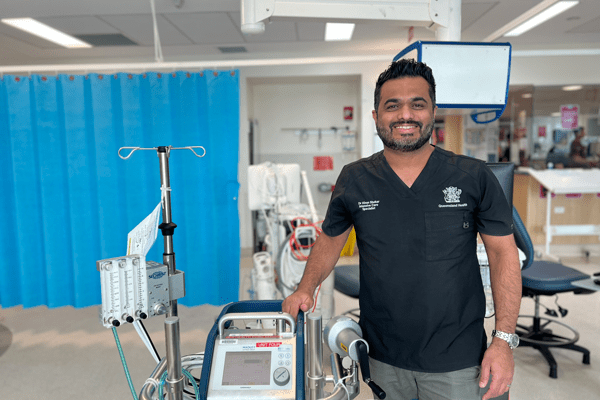
These concerns drove Professor Kiran Shekar, Senior Intensive Care Specialist and Director of Research Professor at The Prince Charles Hospital (TPCH) Adult Intensive Care Services, to undertake vital research to help gather data and develop strategies for providing sedative, analgesic and antibiotic drugs in ECMO.
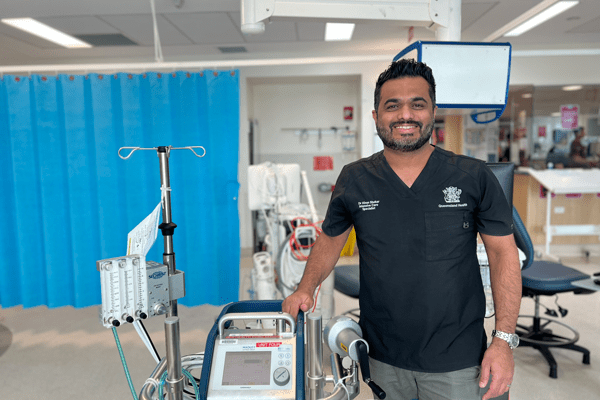
These concerns drove Professor Kiran Shekar, Senior Intensive Care Specialist and Director of Research Professor at The Prince Charles Hospital (TPCH) Adult Intensive Care Services, to undertake vital research to help gather data and develop strategies for providing sedative, analgesic and antibiotic drugs in ECMO.
There is widespread consensus that in hospital, suboptimal dosing of antimicrobials in critically-ill patients leads to treatment failure and microbial resistance which can influence patient outcomes and allocation of resources.
However, is this also true for critically-ill patients on extracorporeal membrane oxygenation (ECMO)?
ECMO is temporary heart-lung bypass that oxygenates a patient’s blood where their own lungs and heart are unable to do so themselves.
However, ECMO is only a supportive therapy that sustains life in critically-ill patients with cardio-respiratory failure. It’s important that the administered drugs, especially antimicrobials, work effectively to contain or reverse the underlying disease so that the patient can be liberated from ECMO and eventually survive.
With ECMO use in adult patients rapidly increasing and evolving following the 2009 H1N1 pandemic, clinicians became increasingly concerned about the effects of pharmacokinetics (PK) or medication-related changes being magnified in critically-ill patients during ECMO. Potential effects included elevated risk of therapeutic failure, drug toxicity and an emergence of microbial resistance.
These concerns drove Professor Kiran Shekar, Senior Intensive Care Specialist and Director of Research Professor at The Prince Charles Hospital (TPCH) Adult Intensive Care Services, to undertake vital research to help gather data and develop strategies for providing sedative, analgesic and antibiotic drugs in ECMO.
Prof Shekar’s globally acclaimed PhD work, the ECMO PK Project, ably supported by the Critical Care Research Group founded by Professor John Fraser, in collaboration with Burns Trauma and Critical Care Research Centre and world PK expert Professor Jason Roberts, aimed to advance comprehensive understanding of PK changes during ECMO.
“ECMO was thought to negatively alter the PK of sedative, analgesic and antibiotic drugs independent of patient and their pathological factors,” Prof Shekar said.
“Our goal was to investigate factors that affect drug PK during ECMO and provide much needed dosing guidance for clinicians globally.”
In addition to mechanistic and studies in bench and animal models, the ECMO PK Project also included an international, multi-centre clinical PK study (ASAP ECMO) that enrolled critically-ill patients admitted to the intensive care units in Australia including TPCH, New Zealand, Switzerland and Republic of Korea. The study was endorsed by the International ECMO Network, a leading platform for global collaborative ECMO research.
“The PK data gathered through the study enabled evidence-based guidance for 18 commonly used antibiotic, sedative and analgesic drug therapies during ECMO,” Prof Shekar said.
“The right dose of the right antibiotic will not only lead to improved microbiological and clinical cure rates in an individual patient, but also will reduce the emergence of multi-resistant organisms.
“Our research reassured clinicians that the independent effect of ECMO on PK is not as highly significant as first feared and current dosing guidelines for critically-ill patients are sufficient for most antimicrobial drugs.
“The ECMO PK project is a testament to how clinicians, scientists, engineers and other key stakeholders in the health system can work collaboratively to understand and solve an important problem we encounter at the bedside.”
Acknowledgement goes to TPCH Adult Intensive Care Service staff and multidisciplinary colleagues, and The Prince Charles Hospital Foundation for their support of the project.
