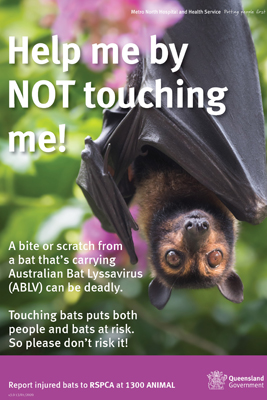
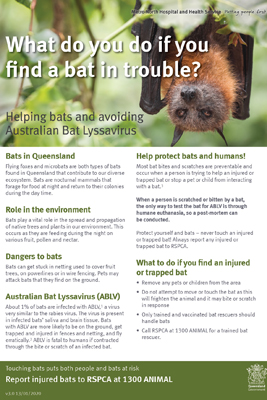
Australian Bat Lyssavirus (ABLV) is a disease similar to rabies which causes a fatal neurological disease in humans.
People who come across an injured bat should contact the RSPCA (1300 ANIMAL), Department of the Environment, Tourism, Science and Innovation (1300 130 372), or local wildlife care groups/rescuers/carers for assistance. Do not touch the bat.
If you have been bitten or scratched by a bat, seek medical advice as soon as possible from your GP, a hospital or call the Metro North Public Health Unit on 3624 1111
Our public health medical officers and nurses work with healthcare professionals in Metro North to assist in the management of potential exposures to ABLV. This is referred to as post-exposure prophylaxis (or PEP). PEP involves a rabies vaccine (+/- rabies immunoglobulin) given before a person becomes unwell to prevent the disease. Clinicians who receive reports of bat bites or scratches are required to notify public health.
Signs and Symptoms
ABLV infection in humans causes a serious illness which results in paralysis, delirium, convulsions and death. Since November 1996, three people have died as a result of ABLV infection, after being bitten or scratched by bats.
Treatment
Rabies vaccine that is given after exposure to ABLV, but before a person becomes unwell, will prevent the disease. However, once a person develops the disease there is no specific treatment for ABLV.
Proper cleaning of the wound reduces the risk of infection. If bitten or scratched, immediately wash the wound thoroughly with soap and water for at least 15 minutes. If available, an antiseptic with anti-virus action such as povidone-iodine or alcohol (ethanol) should be applied after washing. If bat saliva contacts the eyes, nose or mouth, flush the area thoroughly with water for several minutes.
Seek medical advice about the need for rabies vaccination as soon as possible, preferably on the same day or early in the day after the exposure to the bat occurred. A tetanus injection may also be necessary after a bat bite or scratch.
While bat faeces, urine and blood are not considered to pose a risk of ABLV, contact with any bat fluids should generally be avoided. If you have any contact with bat fluids, wash your hands (or other affected area) immediately.
- Rabies and other lyssavirus – CDNA National Guidelines
- Management of potential exposures to Rabies and Australian Bat Lyssavirus
Transmission
The virus can be transmitted from bats to humans when infected bat saliva enters the human body, usually by a bite or scratch, but also by getting bat saliva in the eyes, nose or mouth (mucous membrane exposure) or onto a pre-existing break in the skin.
The virus is also found in the nervous system of affected bats. Therefore needlesticks or cuts from a sharp item that has been used on a bat, or coming into contact with brain tissue from a bat, are also possibly ways of transmitting ABLV.
ABLV is unlikely to survive outside the bat or in a dead bat for more than a few hours, especially in dry environments that are exposed to sunlight. Coming into contact with bat faeces, urine or blood do not pose a risk of exposure to ABLV, nor do living, playing or walking near bat roosting areas. There is no evidence to suggest ABLV could be contracted by eating fruit partially eaten by a bat. However, any fruit that has been partially eaten by any animal should be discarded as it could be contaminated by a variety of germs.
The time from exposure to the virus to the start of symptoms is variable; of the three known human cases of ABLV infection, one became ill several weeks after being bitten by a bat and another became ill more than two years after a bat bite. The timeframe around exposure of the third case is not confirmed. Classical rabies virus also shows a wide variability in time between exposure and illness, from weeks to years. Therefore, it is vital to seek medical advice even if some time has elapsed since the exposure.
Prevention
- Do not touch bats, even if they are injured.
Only vaccinated people who have been trained in the care of bats should ever handle bats or flying foxes. People who come across an injured bat should contact the Department of the Environment, Tourism, Science and Innovation (1300 130 372), RSPCA (1300 ANIMAL) or local wildlife care groups/rescuers/carers for assistance. Do not touch the bat. - Rabies vaccination
Rabies vaccine is used to protect against ABLV infection. Even if a person has had rabies vaccine before, further rabies vaccinations will be required if they are exposed to ABLV.
There are two types of vaccine that may be used:
- Rabies Vaccine contains killed virus that cannot cause the disease. The vaccine stimulates a person’s immune system to develop antibodies that will recognise and kill the virus before it has time to cause illness.
- Human Rabies Immunoglobulin (HRIG) is made from blood donated by people who have been vaccinated against rabies. It is a concentrated form of antibodies against rabies virus. HRIG may be recommended for immediate protection for people who are exposed to ABLV and have never had rabies vaccination before. As much as possible of the HRIG dose is injected around the exposure site, with any remainder given as an injection into a muscle such as the buttock or thigh.